In Hawaiʻi, rat lungworm disease is responsible for many cases of debilitating illness every year sometimes resulting in death. The clinical subcommittee of the state’s Joint Task Force on Rat Lungworm Disease has recently revised the preliminary guidelines for the diagnosis and treatment of rat lungworm disease. Led by Vernon Ansdell, an internist and associate professor at the University of Hawaiʻi at Mānoa John A. Burns School of Medicine (JABSOM), the updated recommendations were published in the journal Parasitology.

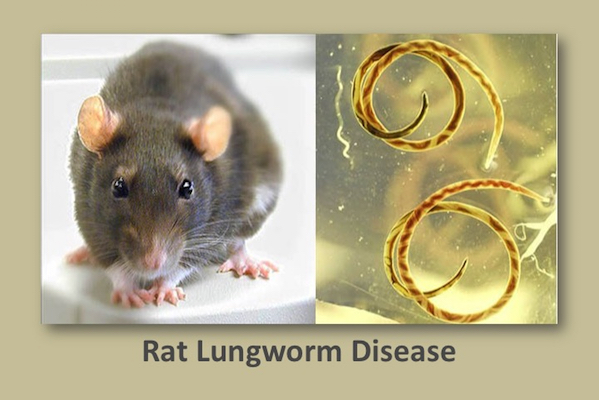
Most people in Hawaiʻi are believed to become infected after eating green leafy vegetables contaminated with slugs or snails infected with Angiostrongylus cantonensis, a nematode worm. Cases of rat lungworm disease appear to be more severe in Hawaiʻi than in other parts of the world, possibly due to recently introduced semi-slugs that often contain large numbers of A cantonensislarvae.
Ansdell says the new guidelines emphasize both early diagnosis and early treatment using high dose corticosteroids to reduce inflammation in the central nervous system, and antiworm treatment with albendazole to kill worms at an early stage before they grow and cause significant damage. In addition, new, more sensitive tests of the cerebrospinal fluid and blood being developed by the National Institutes of Health may help with earlier diagnosis.
“Early diagnosis is very difficult because most cases present with vague, nonspecific symptoms, resulting in significant delays in treatment,” said Ansdell. “Current evidence suggests that early diagnosis and treatment could result in improved outcomes with long-term disabilities and deaths.”.
“We need detailed information on cases in Hawaiʻi as they arise,” Ansdell added. ”Collaborative international clinical research will help us to learn more about the diagnosis and treatment of this challenging disease.”
“Guidelines for the diagnosis and treatment of neuroangiostrongyliasis: updated recommendations,” published in Parasitology in July 2020 includes additional authors Kenton Kramer, Jourdan McMillan, William Gosnell, Gerald Murphy, Olivia Smith and Marian Melish of the UH medical school as well as Drs. B.C. Meyer, Elizabeth Blalock, Johnnie Yates and Louis Lteif. See the online publication at Cambridge University Press.
Dr. Ansdell says the new guidelines emphasize both early diagnosis and early treatment using high dose corticosteroids to reduce inflammation in the central nervous system and antiworm treatment with albendazole to kill worms at an early stage before they grow and cause significant damage. In addition, new, more sensitive tests of the cerebrospinal fluid and blood being developed by the National Institutes of Health may help with earlier diagnosis.
“We need detailed information on cases in Hawaiʻi as they arise,” Dr. Ansdell said. “Collaborative international clinical research will help us to learn more about the diagnosis and treatment of this challenging disease.”
Originally from England, Dr. Ansdell came to Hawaiʻi 40 years ago with a desire to help people and use his background in tropical medicine to work on some of the unusual infectious diseases that occur in Hawaiʻi. He enjoys the collegial atmosphere at JABSOM with talented and dedicated faculty such as his colleagues Drs. Kenton Kramer and William Gosnell. Outside of work, Dr. Ansdell’s favorite local spot is among the clouds on Haiku Stairs on Windward, Oʻahu.
Discussion from Parasitology:
The spectrum of disease caused by A. cantonensis in Hawaii reflects that reported from other regions (Oehler et al., 2014). However, serious illness appears more common in Hawaii and countries such as Australia and Jamaica (Blair et al., 2013; Evans-Gilbert et al., 2014) compared to Thailand, where most of the treatment trials have been conducted. This difference may be due to the inoculum of infectious larvae ingested. In Thailand, aquatic snails and paratenic hosts (which account for the majority of infections) are believed to have relatively lower larval burdens (Eamsobhana, 2014). In contrast, terrestrial gastropods in Hawaii (which are intentionally or inadvertently ingested) may contain enormous larval loads. The disproportionate amount of severe disease in Hawaii and countries such as Australia emphasizes the importance of early diagnosis and treatment of neuroangiostrongyliasis (NAS), prior to the development of serious CNS damage.
NAS poses a significant diagnostic challenge. The gold standard finds the larvae in the CSF or eye but this is rare. Various serological assays have been developed in international reference laboratories (Wilkins et al., 2013); however, none have been validated in the USA. Due to high specificity, RTi-PCR is becoming the gold standard for confirming active infection.
At present, NAS patients are best managed with LPs to reduce ICP and provide headache relief, high-dose corticosteroids to reduce inflammation in the CNS and albendazole to minimize damage from migrating parasites. It should be noted that the effectiveness of albendazole depends on the parasite’s stage of development in the CNS. Based on animal studies, maximum parasite killing occurs during periods of rapid growth, which is 5–14 days after ingestion (Prociv and Turner, 2018). Because parasite death may increase inflammation, albendazole should be given under steroid coverage in symptomatic patients.